Overview
Afya Imara started as a collaboration with the Christian Social Services Commission and Sanofi focused on delivering measurable outcomes through our technology-enabled approach to community-based care. Today, we’re expanding across the faith-based health system while testing novel sustainability models to support scale.

Partners
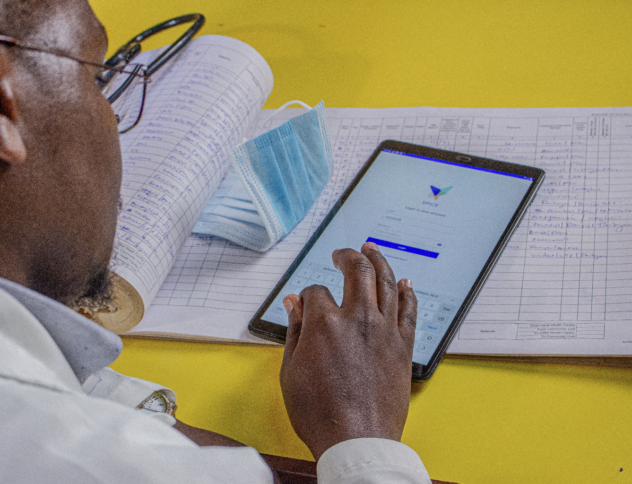
How it works
SPICE, our open-source technology platform, supports outcomes-focused patient care.
SPICE Highlights
Regional Customization
SPICE supports Swahili, among other languages.
Patient Engagement
Health facility staff use SPICE Engage to follow-up with patients via telehealth.
Analytics
SPICE Insights support our partners with data literacy.
Meet SPICE, the technology behind our work
We’re cultivating system-level change through digital health transformation. SPICE is the world’s leading digital health platform for community-based population health.
Our Technology